
By Benjamin Ikegbunam B.Sc., M.Sc. (Reporting Radiographer & Enthusiast, Point-of-Care diagnostic imaging) & Dr Ramdas Senasi MBBS MRCS FRCR (Consultant Radiologist & Public speaker)
Background
Diagnostic imaging services within the NHS hospitals often face significant delays causing important diagnoses and treatments to be put on hold. Patients must travel to these hospitals for x-rays, which can be especially challenging for those who are unable to leave their homes, are frail, or have cognitive impairments. Additionally, visiting hospitals for imaging increases the risk of contracting infections, particularly for at-risk populations. The process of getting an x-ray at an NHS hospital can be both upsetting and inconvenient, not only for the patients themselves but also for their families who may need to take time off work or make travel arrangements. Moreover, NHS hospitals may not always provide immediate radiology reports, potentially causing treatment decisions to be delayed and heightening anxiety for patients.
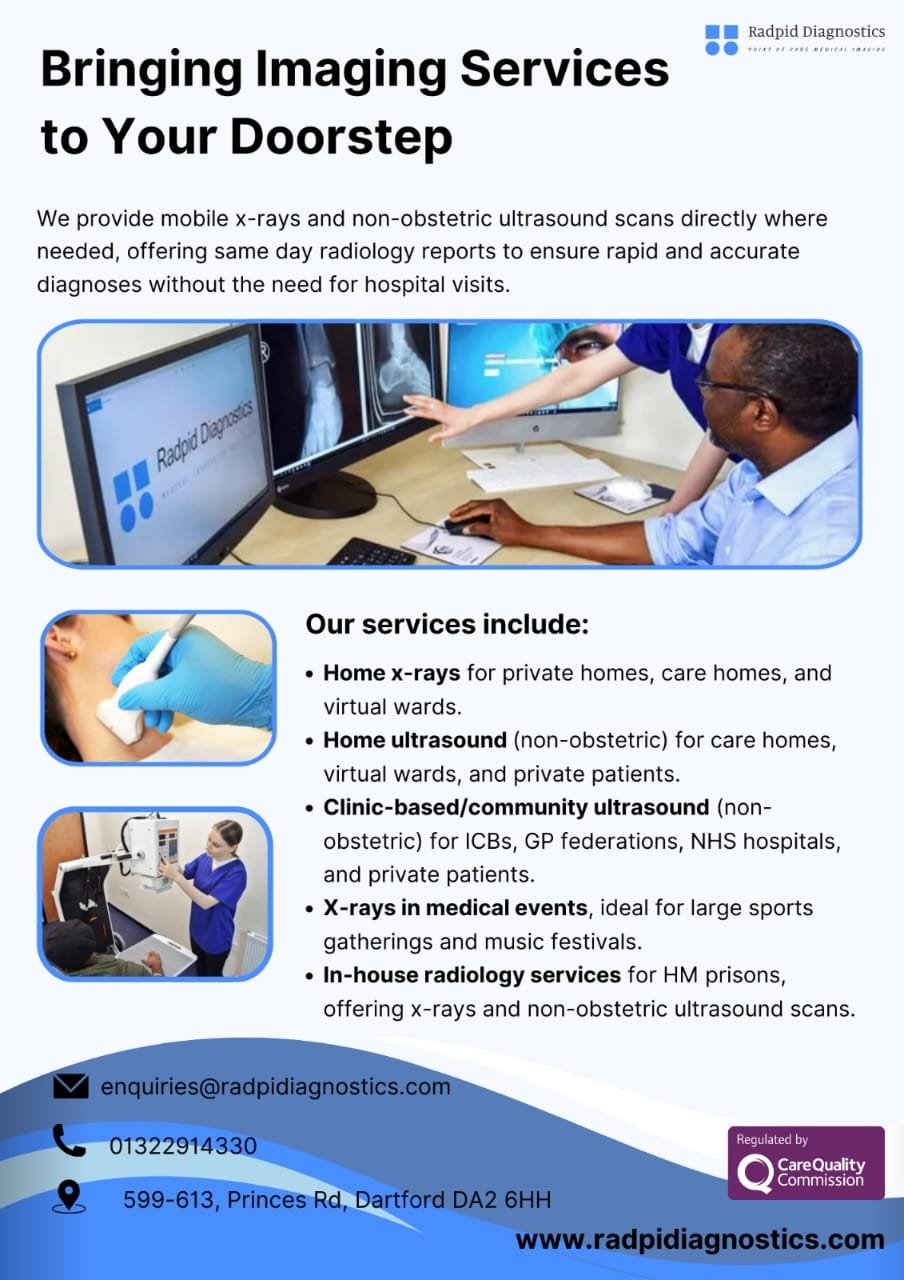
Home x-ray services are a recent development in the UK, although they have been effectively utilized in various other countries including Australia, Canada, Italy, Ireland, Norway, Sweden, and the USA. Implementing these services in the UK could offer significant benefits and alleviate some of the current challenges faced by NHS hospitals.
The Importance of Home X-Rays
Home x-rays offer significant benefits to patients, particularly those who are vulnerable or have difficulty going to the hospital for a test. It eliminates the need for patients to make difficult and potentially hazardous trips to hospitals or medical imaging centres for imaging alone. Instead, mobile diagnostic imaging equipment can be brought to private homes, care homes, and assisted living facilities where most residents are elderly or have disabilities. By providing this service, the risk of further injury and inconvenience to the patients is greatly reduced (Toppenberg et al., 2020).
Transporting care home residents or patients, especially those with memory disorders, to the hospital for radiological examinations can be stressful and disorienting. However, advancements in medical imaging now allow evaluations to be conducted at the point of care (care home facility). This reduces anxiety, eliminates waiting times and non-coordinated ambulance or hoist transfers, increases the number of examinations catered to, and improves timely diagnosis and access to treatments. Portable X-ray devices have been found to eliminate the need for hospital trips, leading to reduced hospitalisations and lower healthcare costs (Dollard et al., 2023).
By offering patients the choice to receive medical care at home or through virtual wards, the number of unnecessary hospital visits will decrease, resulting in cost savings for the NHS. Home X-rays can be useful in tracking the development of certain conditions, enabling treatment plans to be modified more promptly. The convenience and cost efficiency of this approach make it a beneficial tool for enhancing patient outcomes and decreasing unnecessary hospital trips, thereby reducing the risk of post-hospitalisation medical complications (Provencher et al., 2021). In addition, portable X-ray services have demonstrated potential socio-economic benefits. A cost-effectiveness analysis conducted in Norway has indicated that these systems can reduce the dependence on ambulance and taxi services while also providing staff support for residents traveling to and from the hospital. This suggests that portable X-ray systems are a cost-effective solution (Kjelle & Lysdahl, 2017).
Impact on Hospitalisation Rates
The National Health Service (NHS) historically admits patients with chest infections or acute heart failure for diagnostic purposes, resulting in inefficient use of hospital resources in some settings. Chest x-rays are commonly used to diagnose respiratory diseases such as pneumonia. Chest x-rays in primary care settings increase the positive predictive value (PPV) of pneumonia (Adamson et al., 2024), enabling early diagnosis and treatment.
Implementing home X-ray services has shown promising results in reducing unnecessary hospitalisations for elderly patients presenting with low risk of fracture falls/injuries (Hay, 2024) and can potentially lead to significant cost savings for the NHS. The convenience of being able to receive X-rays at home also improves patient satisfaction and overall healthcare outcomes. Additionally, home X-ray services help to alleviate the strain on hospital resources by keeping beds available for more urgent cases.
Cost Savings and Resource Allocation
The shift from showcasing advanced imaging capabilities in nursing and care home environments to broader implementation depends largely on cost-effectiveness. MedTech/Diagnostic imaging companies must tackle this challenge in discussions with decision-makers at NHS England. With the NHS dealing with growing pressure on resources and hospital space, any proof that Care Home x-rays can effectively decrease hospital admissions at a reasonable price would be greatly appreciated. The steep costs of hospital stays are primarily linked to Healthcare-Associated Infections (HCAIs). According to Guest et al. (2020), there were an estimated 653,000 HCAIs among the 13.8 million adult inpatients in NHS general and teaching hospitals in England in 2016/2017, amounting to around £2.1 billion for the year, equating to £586.59 per day for the General ward. This is where home X-rays and other home diagnostic tools could have a significant impact in cutting down on unnecessary hospital stays by detecting and monitoring conditions early, leading to cost savings and improved resource management.
On a separate report, the average expenses for end-of-life care for nursing home residents increases by £4,223 if they pass away in a hospital instead of a care home (Ennis et al., 2015). Statistics from death records reveal that only 22% of older people in Southwest London, with a total of 8,578 beds, died in care homes in 2017 (Health Innovation Network South London, 2019). By preventing 100 of such hospital deaths through the implementation of home diagnostic services like home X-rays, there could be cost savings of about £422,300 and better allocation of resources in healthcare. Not only would this decrease unnecessary hospital visits, it would also allow individuals to pass away in their desired setting with dignity and comfort. Shifting towards the use of home X-rays for diagnostics could transform the healthcare system and enhance patient outcomes. Hence, incorporating home X-rays and other home diagnostic methods could play a crucial role in reducing needless hospitalisations and provide a cost-effective healthcare solution in the UK.
Conclusion
We have seen the number of unnecessary hospital admissions in NHS Trusts and the increasing cost for treatment. Early detection and treatment of certain health conditions, such as chest infections, within care homes can greatly reduce the need for hospitalization. Additionally, the use of non-hospital x-rays can reduce the occurrence of unnecessary hospitalisation by excluding fractures at the point of care in several at-risk groups.
This highlights the importance of implementing home X-ray services in primary care settings to further prevent unnecessary admissions and improve patient outcomes. By utilizing this home imaging technology, healthcare providers can effectively monitor and diagnose patients in a timely manner, ultimately leading to a more efficient healthcare system. This helps residents maintain health and independence, preventing admissions to hospital. In conclusion, the implementation of home X-rays has the potential to significantly reduce the number of unnecessary hospitalizations in NHS hospitals.
Call to Action
To realize these benefits, it is crucial for policymakers, healthcare providers, and stakeholders to support the integration of home X-ray services into the NHS. Pilot programs, funding allocations, and partnerships with mobile imaging companies should be prioritized. This proactive approach can enhance patient care, reduce costs, and optimize resource allocation within the NHS.
References:
Adamson, A.J., Kallis, C., Douglas, I., and Quint, J.K. (2024). Accuracy of the recording of pneumonia events in English electronic healthcare record data in patients with chronic obstructive pulmonary disease. Pneumonia. Available at: https://springer.com (Accessed: 27 May 2024).
Dollard, J., Edwards, J., Yadav, L., Gaget, V., Tivey, D., Maddern, G.J., and Visvanathan, R. (2023). Mobile X-ray services in nursing homes as an enabler to healthcare-in-place for residents: informal carers’ views. BMC Geriatrics, 23(1), p.458. Available at: https://springer.com (Accessed: 27 May 2024).
Ennis, L. et al. (2015). The cost of providing end of life care for Nursing Care Home Residents: A retrospective cohort study. Health Services Management Research, 28(1–2), pp. 16–23. doi:10.1177/0951484815607541.
Guest, J.F. et al. (2020). Modelling the annual NHS costs and outcomes attributable to healthcare-associated infections in England. BMJ Open, 10(1). doi:10.1136/bmjopen-2019-033367.
Hay, K. (2024). Fewer people go to hospital due to Cornwall home X-ray trial – GP, BBC News. Available at: [Link] (Accessed: 27 May 2024).
Health Innovation Network South London (2019). Southwest London STP – Care Home Data Pack. Available at: [Link] (Accessed: 27 May 2024).
Kjelle, E. and Lysdahl, K.B. (2017). Mobile radiography services in nursing homes: A systematic review of residents’ and societal outcomes. BMC Health Services Research. Available at: [Link] (Accessed: 27 May 2024).
Provencher, V., D’Amours, M., Menear, M., Obradovic, N., Veillette, N., Sirois, M.J. and Kergoat, M.J. (2021). Understanding the positive outcomes of discharge planning interventions for older adults hospitalized following a fall: a realist synthesis. BMC Geriatrics, 21, pp.1-18. Available at: https://springer.com (Accessed: 27 May 2024).
Toppenberg, M.D., Christiansen, T.E.M., Rasmussen, F., Nielsen, C.P. and Damsgaard, E.M. (2020). Mobile X-ray outside the hospital: a scoping review. BMC Health Services Research, 20, pp.1-12. Available at: https://springer.com (Accessed: 27 May 2024).






Hey people!!!!!
Good mood and good luck to everyone!!!!!